Physiotherapy after ACL reconstruction is, honestly, the real backbone of getting your knee back to normal. If you skip proper rehab, even the best surgery in the world won’t get you all the way there—physiotherapy is what actually brings back your strength, flexibility, and movement. We get it: recovery isn’t just about fixing a torn ligament. It’s about rebuilding your knee’s stability and the way it moves, so you can trust it again.
Those first weeks and months after surgery are all about targeted exercises and hands-on therapy. They help keep swelling down, make pain manageable, and stop your knee from getting stiff. We like to keep things gradual, adjusting to each person’s needs—there’s no one-size-fits-all plan here. That way, we can keep an eye on your healing, but also nudge you back into safe activity. Stick to expert advice and a solid physio routine, and your odds of a smooth return to normal life go way up.
Working with someone experienced, like Dr Sandeep Singh, really makes a difference. He’s big on personalised care and exercise plans that actually fit your situation. That’s why physiotherapy isn’t just a box to tick; it’s the key to moving forward with confidence. If you want more in-depth tips, check out Dr Singh’s advice over on the Dr Sandeep Singh ACL surgery blog.
Understanding ACL Reconstruction and Its Purpose
What Is the Anterior Cruciate Ligament?
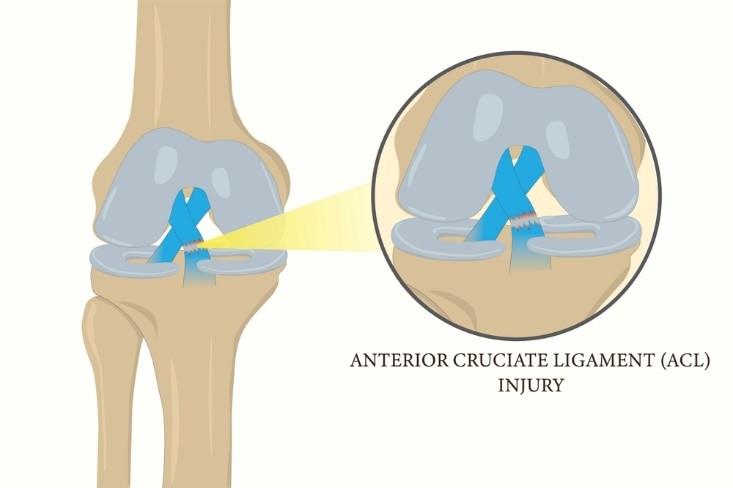
The anterior cruciate ligament (ACL) is one of four main ligaments holding your knee together. It connects your thigh bone (femur) to your shin bone (tibia), and its main job is to keep the knee steady, especially when it comes to forward movement and twisting.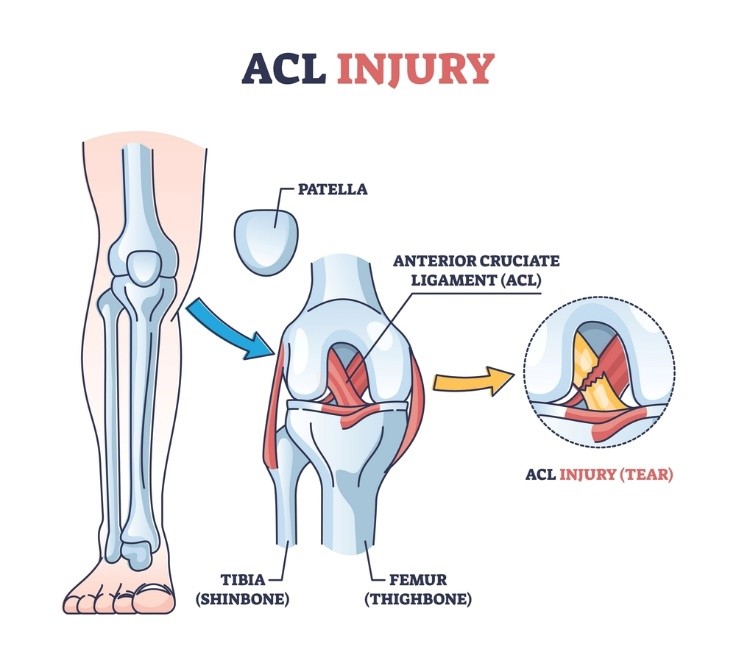
The ACL’s crucial for stuff like running, jumping, or just changing direction quickly. If you injure your ACL, you’ll probably notice your knee feels unstable—sometimes it even gives way. That can make everyday movement tough, let alone sports. Knee instability is no joke.
Because it sits right inside the knee joint, the ACL can take a beating in sports or accidents. Without it working properly, your knee can move in weird ways, which just increases the risk of damaging cartilage or other ligaments down the line.
Why Is ACL Surgery Necessary?
So, when does surgery come into play? Basically, if the ACL is torn and your knee is wobbly enough to mess with your day-to-day or sports, then surgery is usually recommended. Sure, physio helps, but it can’t magically knit the ligament back together or fully restore joint stability.
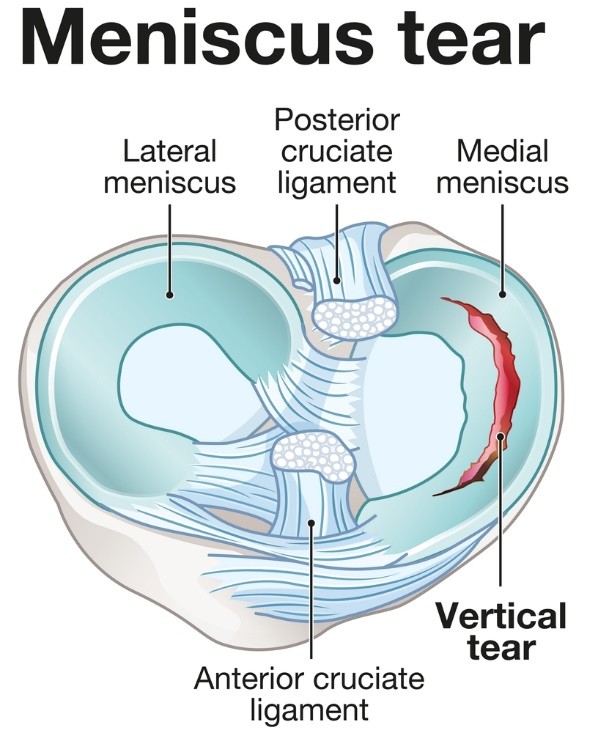
If you don’t get it fixed, that ongoing instability can lead to meniscus tears and, honestly, early arthritis. Surgery aims to get your knee working right again and prevent more damage.
We tend to push for surgery in younger, active folks who want to get back to sports or tough physical jobs. The surgical plan and what you do after are both essential for a good outcome and to avoid setbacks.
Types of ACL Reconstruction
There are really two main ways surgeons rebuild the ACL, depending on where the graft comes from:
- Autograft: The tissue comes from your own body—usually your patellar tendon, hamstring, or sometimes the quadriceps tendon. This option lowers the odds of rejection.
- Allograft: The tissue is donated from someone else (a cadaver). It can make the surgery a bit quicker and you’ll have less pain where the graft is taken from, but there’s a slightly higher risk it won’t hold up as well over time.
The choice depends on your age, activity level, and what your surgeon thinks is best. Surgery is done arthroscopically these days, which means small cuts and special tools for precise graft placement and fixation.
Knowing about these options helps you get ready—not just for the operation, but also for rehab and what to expect as you get back on your feet. For more nitty-gritty on treatment and physiotherapy after ACL reconstruction, check out the guide at Physiotherapist India.
Role of Physiotherapy After ACL Reconstruction
Physiotherapy is honestly the unsung hero after ACL reconstruction—it’s what gets your knee working and feeling stable again. It’s all about regaining strength, getting flexible, knocking down pain, and staying ahead of complications. Rehab isn’t one-size-fits-all; it’s adjusted as you heal and based on what you need most.

Importance in Recovery
Right after surgery, physio is key for keeping swelling down and pain under control. Early movement is important to stop your knee from getting stiff. We usually start with gentle exercises to wake up the muscles around your knee, but nothing that risks the new graft. As you get further along, physio helps you walk normally and keeps your balance in check. That way, you don’t end up with weird compensations or overloading the wrong parts of your body. If you try to go it alone, you risk ending up with a stiff or unstable knee—and that just slows everything down.
Benefits for Long-Term Knee Health
Good physiotherapy is also about the long game. It helps rebuild your quads and hamstrings, which are your knee’s main support crew. Strong muscles protect your new ligament from unnecessary stress. Plus, sticking with therapy lowers your chances of re-injury or developing arthritis later on. By working on flexibility and neuromuscular control, physio helps you move better—whether you’re playing sports or just doing daily stuff. Fixing the way you move can even prevent the same kind of injury from happening again. Honestly, keeping up with physio is what keeps your knee feeling good in the long run.
Goals of Rehabilitation
Our main goals? Get you moving pain-free, restore your range of motion, and build up muscle strength so your knee feels stable again. We set small milestones—like bending and straightening your knee without pain, then moving on to putting weight through it and activating the right muscles. We also work on proprioception—that’s your knee’s sense of position—because that’s what keeps you from rolling your ankle or stumbling. Once you’re strong and stable, we’ll start adding in sport-specific drills or whatever functional tasks your life demands. Everyone’s timeline is different, but these goals are what get you back to normal after ACL surgery. If you want a deeper dive into the rehab process, Dr. Sandeep Singh explains it well in his piece on the role of physical therapy after robotic-assisted knee surgery.Dr. Sandeep Singh’s Approach to Post-Operative Rehabilitation

After ACL reconstruction, our focus is to lay out a structured, evidence-based rehab plan that actually works for each stage of recovery. We’re all about steady healing, rebuilding mobility, and getting you strong enough to avoid another injury. Education and support are baked into this process—patients who know what’s going on tend to stick with the plan better.
Initial Assessment and Care Plan
First up, we do a thorough check: how’s your knee moving, how bad is the swelling, what’s your pain like, and what’s your overall health status? This helps us tailor the plan to you, not just some generic protocol. Early movement is encouraged, but only as much as is safe for the new graft.
At the start, it’s all about controlling swelling—ice, compression, and keeping that leg up. Gentle range-of-motion exercises come in early, but we’re careful not to push too hard. We also check your baseline muscle strength so we can track progress as you go.
We like to set clear, realistic milestones. These markers help us know when to move you to the next stage, making sure we don’t rush things and risk the new ligament.
Monitoring Progress and Adjustments
Regular follow-ups are a must. We look for improvements in strength, flexibility, and stability using clinical tests and, honestly, just listening to how you feel. If we spot any issues—maybe swelling that won’t quit or pain that seems off—we tweak the plan right away. We ramp up exercise intensity and type as your knee heals. For example, you’ll put more weight on it as the graft gets stronger. Functional movements get more attention too, so you’re ready for daily life (and eventually, sports) when the time’s right. We also start proprioception and neuromuscular training as soon as you’re ready. This helps your knee learn to “feel” again, which is huge for injury prevention down the road.Patient Education and Support
Teaching patients about what’s happening after ACL surgery is a big part of successful rehab. We talk about why sticking to your exercises matters, and what kind of recovery timeline is realistic—managing expectations is half the battle. We also show you what warning signs to watch for, like swelling that won’t go away or pain that feels wrong. Mental support is part of the package too, since frustration and anxiety are pretty common on this journey. Keeping a positive attitude and staying motivated really help. We’ll also give lifestyle tips—like why quitting smoking is a good idea—since those things can affect how well you heal after ACL reconstruction.If you want to see more about how this is done, check out Sandeep Singh’s approach to ACL rehab.
Phases of Physiotherapy After ACL Reconstruction
Rehab after ACL surgery isn’t just a straight line—it’s a series of phases, each building on the last. The main goal? Protect the new graft, and slowly bring back your knee’s movement, strength, and function. Step by step, you get closer to handling daily life and, if you’re aiming for it, getting back to sports.
Early Rehabilitation (0–6 Weeks)
In the beginning, it’s all about keeping the graft safe and managing pain and swelling. Usually, your knee is kept straight with a brace for the first couple of weeks. You’ll start putting some weight on it soon after surgery, using crutches to help you get around on your own.
We focus on getting full knee extension back and gently working on bending, with exercises like heel slides or assisted knee bends. Activating your quads is super important to stop muscle loss—think static contractions and straight leg raises. To keep swelling down, we stick to the RICE routine: rest, ice, compression, and elevation.
Patellar mobilisation is a must to avoid stiffness. And just a quick tip: don’t put a towel under your knee, as it can force it into a bent position you don’t want. This phase is strict about what you can and can’t do, but it lays the foundation for good neuro-muscular control later.
Strengthening and Mobility (6–12 Weeks)
Once the graft is healing, we start cranking up the difficulty. Closed-chain exercises—like mini squats, step-ups, and bridges—become the focus for rebuilding your quads, hamstrings, and hip muscles.
By week 12, your range of motion should be nearly back to normal, with stretching and joint mobilisations helping out. We add balance and proprioception work, starting with basic single-leg stands and working up to dynamic moves on unstable surfaces.
Stationary cycling is great for improving knee mobility without putting too much stress on your knee. If needed, we might use electrical stimulation to help wake up your quads. Progress is always gradual—we’re careful not to overload the graft or risk instability.
Advanced Functional Training (3–6 Months)
At this point, the focus shifts more toward endurance and dynamic control, and we start mixing in higher-intensity strengthening with more cardiovascular work. Functional moves—think lateral lunges, single-leg squats, step-downs—are key for retraining movement patterns and shoring up joint stability.
Agility drills and carefully controlled plyometrics come into play now, aiming to mimic the demands of whatever sport or activity you’re itching to get back to. Swimming and using the elliptical are great options for low-impact cardio that still keeps your fitness up.
We keep a close eye on knee swelling, pain, and function, dialing intensity up or down as needed. Honestly, this stage takes a lot of discipline—neuromuscular retraining is no joke if you want to be truly ready for tougher activities later.
Return to Sport and Full Activity

Usually, around 6 to 9 months after surgery, the conversation shifts to returning to sport or work. Running gets the green light only when your quadriceps strength is at least 80% of your other leg—no shortcuts here.
Drills ramp up in speed, agility, and complexity, always with supervision. Plyometrics and skills specific to your sport become the main focus, making sure you’re really ready. And yeah, keeping up with strength and flexibility is non-negotiable if you want to avoid setbacks.
Functional testing helps guide the decision to return fully. We can’t stress enough how important it is to ease back into competition, keeping technique sharp and always watching for pain. For most folks, a full recovery takes about 9 to 12 months—sometimes a bit longer, sometimes less, but patience pays off.
If you want to dive deeper into physiotherapy protocols after ACL reconstruction, check out physiosunit.com.
Essential Exercises and Techniques in Rehabilitation
Rehab after ACL reconstruction isn’t just about grinding through exercises—it’s about targeting the right ones to rebuild strength, movement, and stability. We aim to get muscles firing early, keep knee flexibility up, and retrain balance to protect your new ligament and make recovery smoother.
Straight Leg Raises and Quad Sets
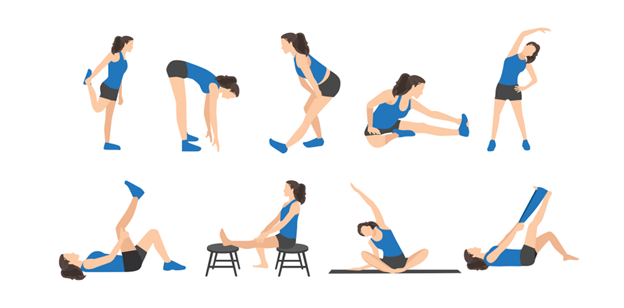
Range of Motion and Flexibility

Balance and Proprioception Activities

Balance work is a big deal because the injury and surgery mess with how your body senses joint position (proprioception). That’s something you don’t want to skip.
Early on, it’s just single-leg stands on solid ground. As things improve, we add unstable surfaces—balance boards, for example—to keep challenging control. These drills sharpen coordination and cut down the odds of re-injury, retraining muscles to react fast during movement.
Common Challenges and How to Overcome Them
Managing Swelling and Pain
Swelling and pain? They’re pretty much guaranteed after ACL surgery. Both can lock up your knee and stall progress if you don’t get on top of them. We jump on early intervention—ice, elevation, compression—anything to keep inflammation down. Gentle manual therapy can loosen up stiffness around the joint. Controlled pain management is key too; you want to be able to do your exercises without making things worse. It’s a balancing act, and keeping tabs on swelling helps avoid setbacks with range of motion. Some go-to practices for swelling and pain:- Frequent icing, especially after rehab sessions
- Keeping your leg up above heart level
- Compression sleeves or bandages
- Gentle mobilization from your physio
Addressing Muscle Weakness
Muscle weakness, especially in the quads and hamstrings, is just part of the deal after ACL surgery. It’s mostly down to disuse and the trauma from surgery itself. Getting those muscles strong again is non-negotiable if you want your knee to work right. We start with low-load, activation-focused exercises to wake up the muscles without putting the graft at risk. As you get stronger, we crank up the intensity to build strength and endurance. Weight-bearing and dynamic moves come in gradually. Throughout, we’re sticklers for good technique—no cheating or weird compensations, since those can just cause more problems. How we tackle muscle weakness:- Begin with isolated activation like quad sets
- Move on to functional exercises—partial squats, step-ups, that sort of thing
- Bring in sport-specific drills before you actually return to play
- Regular check-ins to tweak the program safely
Preventing Loss of Range of Motion
Keeping (and regaining) full range of motion is a constant battle after ACL surgery. Stiffness can sneak up fast if you don’t move the knee enough, and it’ll slow down everything else. We focus on early, supervised movement—enough to avoid stiffness but not so much that you mess up the graft. Gentle manual therapy helps keep scar tissue from taking over and improves circulation around the joint. Stretching is all about restoring extension and flexion, but we’re careful not to push into pain. Good alignment during movement is key—otherwise, you might end up with a limp or other joint issues. We keep a close watch to make sure ROM keeps improving. Some practical strategies for ROM:- Start passive and active-assisted motion ASAP after surgery
- Manual therapy to help with joint mobility
- Slow, steady stretching routines with professional guidance
- Avoid long periods of immobilization unless absolutely necessary
If you want more tips on handling post-ACL rehab challenges, take a look at ClearCut Ortho’s guide to overcoming common ACL reconstruction rehab challenges.

